- Home
- Dr Sultan Linjawi
Type 1 Diabetes
Type 2 Diabetes
Prediabetes
Gestational Diabetes
- Diabetes Information
- Testimonials
GESTATIONAL DIABETES
What is gestational diabetes?

Treating gestational diabetes can greatly improve pregnancy outcome, for both mother and child. For many women, they’re able to achieve normal blood glucose levels through diet alone, however some women may require medications.
What is gestational diabetes?
Gestational diabetes explained simply
Elevated blood sugars often occur in pregnancy and are commonly caused by gestational diabetes (GDM). Mothers with Type 1 diabetes and Type 2 diabetes are also likely to have elevated sugars when pregnant. Around 1 in 5 pregnant women (20%) develop gestational diabetes.
Gestational diabetes explained in detail
In pregnancy there many hormonal changes that occur in the mother in order to facilitate the growth of a baby. Many of these changes are caused by hormones produced by the placenta. Some of these hormones cause the mother’s insulin receptors to become resistant to insulin. Insulin is a chemical that acts like a key, and when bound to the insulin receptor on a cell surface, opens a lock or channel so that glucose can move from the blood into the cells.
If a person is insulin resistant, then they require more insulin to open the lock and transport glucose out of the blood and into the cell. This is the same process that causes type 2 diabetes.
Gestational Diabetes Content |
|---|
| Gestational Diabetes Program |
| Overview |
| Risk Factors |
| Symptoms |
| Diagnosis |
| Complications |
| Treatment |
| Diet |
| Monitoring |
| Tools |
| Mental Health |
| Prevention |
As the placenta grows during the pregnancy, more and more hormones are made and released to support the growth of the baby. This makes the mother more and more insulin resistant. At some point the mother may not be able to produce enough insulin to overcome the resistance, and if this occurs blood glucose levels rise.

High glucose levels readily cross the placenta and expose the baby to sugars that are in the diabetes range, which can cause complications for the baby.
Can gestational diabetes happen to me?
All pregnant women may experience impaired glucose tolerance during pregnancy due to the hormones produced during pregnancy. Most pregnant women are able to make enough insulin to overcome the insulin resistance, but some cannot. For these women, gestational diabetes occurs when the pancreas can't increase the beta cell insulin production function sufficiently to overcome any insulin resistance associated with pregnancy.
Gestational diabetes often develops in pregnant women around the 24th to 28th week of pregnancy. This means that all pregnant woman should be tested for gestational diabetes at 24-28 weeks of pregnancy (except for those women who already have diabetes). Woman at high risk of developing gestational diabetes may have high sugars earlier in the pregnancy.
Typically, gestational diabetes goes away after the baby is born. However, women with gestational diabetes have a greater chance of developing type 2 diabetes later in life. 50% of women with gestational diabetes are likely to go on to develop type 2 diabetes in the future.
Children born to mothers with gestational diabetes, also have a higher chance of developing type 2 diabetes later in life. You can read more about genetics and type 2 diabetes for more information about how our genes can increase our risk of developing type 2 diabetes.
Gestational diabetes develops in pregnant women around the 24th to 28th week of pregnancy. This means that all pregnant woman should be tested for gestational diabetes at 24-28 weeks of pregnancy (except for those women who already have diabetes).
How common is gestational diabetes?
The number of women living with diabetes is increasing. The prevalence of gestational diabetes is related to the prevalence of type 2 diabetes (The Increasing Prevalence of Diabetes in Pregnancy). This means, that as the number of people with type 2 diabetes increases, so does the number of cases of gestational diabetes.
The International Diabetes Federation estimated that in 2017:
- 204 million women aged 20-79 years, have diabetes. This number is set to increase to 308 million by 2045
- 1 in 3 women of reproductive age lives with diabetes
- 21.3 million (16.2%) of live births had some form of hyperglycaemia in pregnancy. It was estimated that 85.1% were due to gestational diabetes
- 1 in 7 births were affected by gestational diabetes
- Hyperglycaemia in pregnancy is mostly prominent in low- and middle-income countries where maternal care is limited
What are the risk factors for developing gestational diabetes?
Every pregnant woman is at risk of developing gestational diabetes, so it is recommended that all pregnant women are screened using a glucose tolerance blood test at 24-28 weeks’ gestation.
There are some women who are at a much higher risk and should be screened before becoming pregnant, at 12 weeks’ gestation and again at 24-28 weeks if not previously diagnosed.
There are a number of risk factors that increase your likelihood of developing gestational diabetes. Like with type 2 diabetes, extra weight is linked to gestational diabetes. This means that women who are overweight or obese, may already have insulin resistance before they become pregnant. Gaining too much weight during pregnancy can also increase the risk of developing gestational diabetes.
Other high-risk factors for developing gestational diabetes include:
- women aged 25 years or over
- family history of type 2 diabetes
- family history of gestational diabetes, especially from a first-degree relative like a mother or sister
- being overweight or obese
- had gestational diabetes in a previous pregnancy
- multiple pregnancies in the past
- have previously given birth to a large baby (weighing more than 4.5kgs)
- gained weight rapidly during the first trimester of pregnancy
- a previous diagnosis of Polycystic Ovary Syndrome
- of non-Caucasian descent, including African-American, Aboriginal or Torres Strait Islander, Melanesian, Polynesian, Chinese, Southeast Asian, Middle Easter or Indian background

Screening for gestational diabetes - how do doctors know when to test for gestational diabetes?
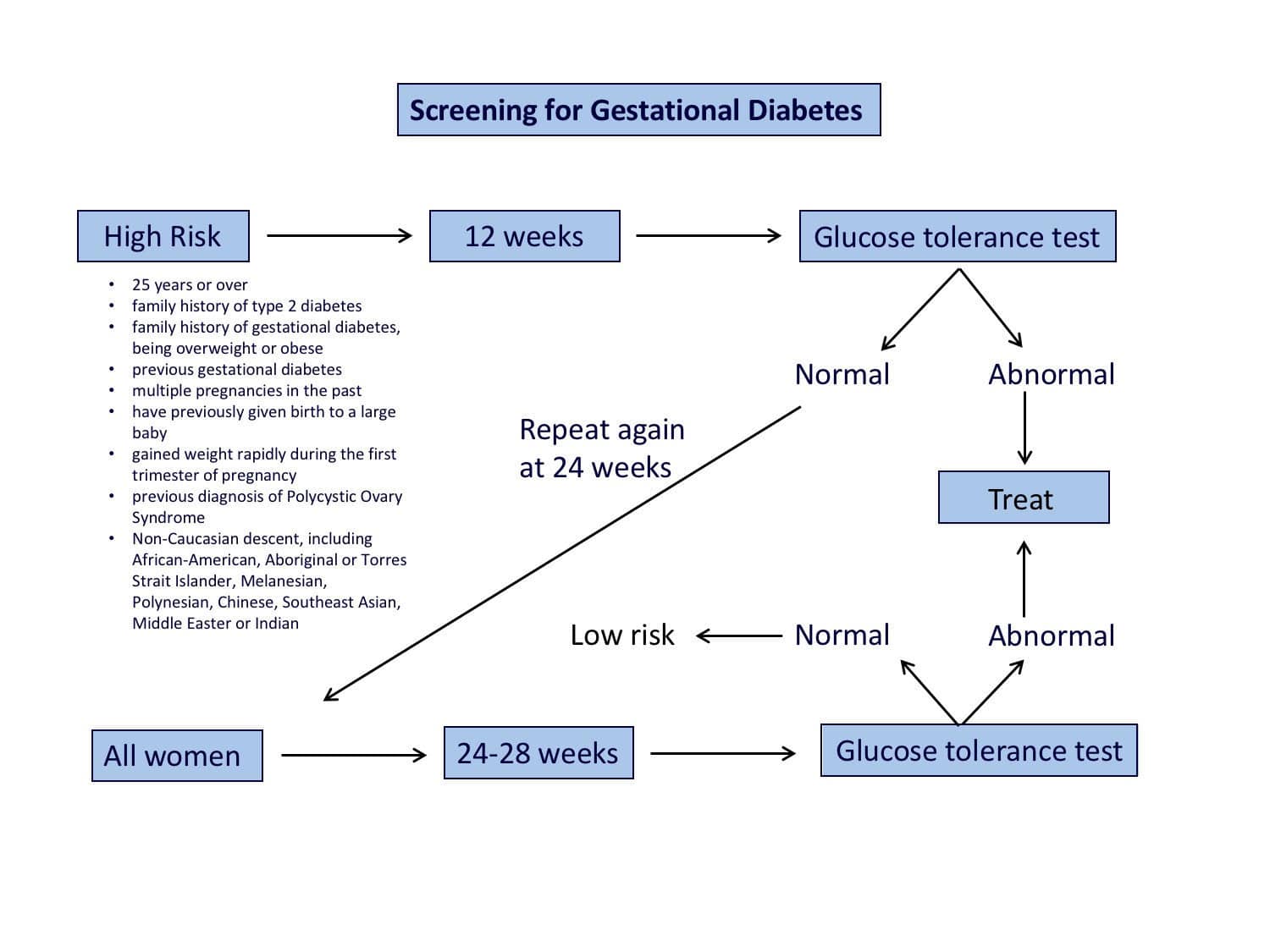
The image below provides an overview of screening for gestational diabetes.
How do you test for gestational diabetes?
All women should be tested for gestational diabetes at weeks 24-28 gestation, which is during the second trimester. If a woman is at a high risk of gestational diabetes such as being overweight at the beginning of your pregnancy; have previously had gestational diabetes; or a close family member (i.e. mother, father, or sibling) has diabetes, your doctor is likely to screen you earlier for gestational diabetes.
A pregnancy oral glucose tolerance test involves:
- fasting overnight (for at least 8 hours)
- initial blood test to test fasting glucose levels
- drinking a syrupy glucose solution containing 75 grams of glucose
- have a blood glucose test at 1 hour after drinking the glucose solution
- have a final blood glucose test 2 hours after drinking the glucose solution
The diagnosis of gestational diabetes is confirmed on high sugar readings at any of the following time points:
- fasting glucose value
- 1 hour glucose value
- 2 hour glucose value
What are the diagnostic criteria for gestational diabetes?
An elevation in blood glucose levels are diagnostic at either the fasting, 1 hour or 2-hour test. You only need one test to show abnormal blood glucose readings higher than normal values for each time point, to be diagnosed with gestational diabetes.
| Fasting glucose | 1 hour glucose | 2 hour glucose |
|---|---|---|
| 5.2 mmol/L or more | 10.0 mmol/L or more | 8.5 mmol/L or more |
| 92 mg/dL or more | 180 mg/dL or more | 153 mg/dL or more |
Read about how diabetes is diagnosed for more information.
What are the glycaemic targets in gestational diabetes?
Currently, there have been no studies that have defined the optimal glycaemic targets for women with gestational diabetes. Further research is required to determine optimal blood glucose targets.
Below are suggested from the Australasian Diabetes in Pregnancy Society targets for women with gestational diabetes:
- fasting blood glucose: 5.0mmol/L (90mg/dL) or less
- 1 hour after eating a meal: 7.4mmol/L (134mg/dL) or less
- 2 hours after eating a meal: 6.7mmol/L (120mg/dL) or less
Your specific blood glucose targets may be set by your doctor if you have type 1 diabetes but generally as close to these values is crucial to reduce complications from gestational diabetes on the mother and baby.
What are the complications associated with gestational diabetes?
Gestational diabetes has been found to be associated with both short-term complications and long-term complications to both the mother and child. It is vital to maintain blood glucose levels as near normal as possible throughout the pregnancy to minimise complications. Safely controlling sugars minimises the chance of complications from happening.
It is important to remember that the complications of gestational diabetes are different to the complications of type 2 diabetes.
How does gestational diabetes affect the mother?
Gestational diabetes can increase the risk of developing the following complications in the mother:
- Difficult delivery. In gestational diabetes, the baby is more likely to be a large baby due to excessive weight. This can result in having a caesarean section or a forceps delivery, which may be distressing for those mothers who wanted to have a natural birth.
- High blood pressure and pre-eclampsia. Gestational diabetes increases the risk of high blood pressure, as well as a condition called pre-eclampsia. Pre=eclampsia is a dangerous condition which refers to the onset of high blood pressure and evidence of organ dysfunction occurring in the later stages of pregnancy (after 20 weeks gestation). It can lead to severe life threatening seizures.
The organs that can be affected include the kidneys, liver, lungs, and brain. Pre-eclampsia can also occur for the first-time during delivery. Preeclampsia can be life threatening to both mother and baby. - Future type 2 diabetes or gestational diabetes. In women who have had gestational diabetes, they are at an increased risk of developing gestational diabetes again for any future pregnancies. You are also more likely to develop type 2 diabetes as you get older. Healthy lifestyle choices can help to minimise the risk of gestational diabetes and type 2 diabetes. Leading a healthy lifestyle following pregnancy, can reduce the development of type 2 diabetes by 50% or more (to Prevention of Type 2 Diabetes in Women With Previous Gestational Diabetes).
How does gestational diabetes affect the baby?
Complications that can happen to the baby include being bigger at birth with the associated risks of a delivery from a large baby. Babies are also likely to be more immature and can experience breathing difficulties after birth and very low blood sugar levels. In the long term a child exposed to high blood sugar levels during gestation is more likely to be overweight and develop diabetes once an adult.
- Increased birth weight. Excessive birth weight, also referred to as large for gestational age, occurs due to increased glucose in your bloodstream crosses the placenta. This causes your baby’s pancreas to start producing extra insulin, resulting in the baby growing too large. Very large babies, weighing 9 pounds (4kgs) or more, can become stuck in the birth canal, causing injuries to you or require an emergency C-section.
- Early birth and respiratory distress syndrome. High blood glucose levels may increase the risk of a mother experiencing early labour and delivering the baby before the due date. Babies that are born too early may experience respiratory distress syndrome, which is a condition that makes breathing difficult, and require assistance breathing. Babies born to mothers with gestational diabetes, could experience respiratory distress syndrome without being born early (Management of Infants of Diabetic Mothers).
- Hypoglycaemia (low blood glucose). Some babies of mothers with gestational diabetes, may experience low blood glucose levels shortly after birth if their own insulin production is too high.
- Type 2 diabetes later in life. Babies are at an increased risk of developing type 2 diabetes later in life, if their mother had gestational diabetes (Short- and long-range complications in offspring of diabetic mothers).
How is gestational diabetes treated?
If you have gestational diabetes, it is important to regularly monitor and control your blood glucose levels to keep you and your baby healthy. This is important, as it can help you to avoid any complications for you and your baby during pregnancy and delivery, as well as later in life.
The preferred method of managing gestational diabetes is through lifestyle management, such as diet and exercise. For some women, they may be required to take medications in pregnancy, for example metformin or insulin. Metformin is a common drug recommended for gestational diabetes, which studies have shown may to be safe for use in pregnancy. It is likely that 30-50% of women with gestational diabetes will require short term insulin to achieve excellent and safe sugar levels.
Healthy diet
Any recommended changes to the diet are based around optimal nutrition for the mother and infant, and controlled weight gain. Like with a type 2 diabetes diet, eating the right types of food during pregnancy can help to control your blood glucose levels and avoid excess weight gain.
A mother needs to eat enough carbohydrates to prevent ketones developing but not too much that it puts too much glucose into the circulation
Women with gestational diabetes need to eat a balanced diet that contains nutrients from all food groups. It is best to completely avoid a keto diet as this may be seriously harmful for the baby. The best diet involves eating a little of everything but not too much. Diabetes and diet in pregnancy is a helpful article outlining what to eat.

Exercise
Regular physical activity plays a key role in before, during, and after pregnancy. Exercise is very beneficial in aiding with controlled weight. Exercise is able to lower blood glucose levels by increasing your cells’ sensitivity to insulin. This means your body needs to produce less insulin to transport glucose from the blood stream and into your cells.

Blood glucose monitoring
Your doctor or endocrinologist may ask you to check your blood glucose levels regularly throughout the day, including when you first wake up in the morning fasting, and after you eat your meals at either 1 hour or 2 hours after eating. This is to make sure that your blood glucose levels are staying in a safe range.
You can test your blood glucose levels with a blood glucose meter by placing a drop of blood on a test strip. You can use a lancet (a small needle) to produce a drop of blood. Once the blood is applied to the test strip, it is then inserted into the blood glucose meter, which will display your blood glucose reading.

Does gestational diabetes go away after delivery?
Generally, most cases of gestational diabetes disappear after pregnancy. This however does need to be confirmed 6-10 weeks after delivery with another 2-hour glucose tolerance test.
50% of mothers with gestational diabetes will go on to develop type 2 diabetes later in life and this is more likely if the correct lifestyle changes are not undertaken. Type 2 diabetes may develop immediately after the pregnancy or many years later. Mothers with gestational diabetes should have yearly or 2nd yearly screening for type 2 diabetes for the rest of their life.
If a mother with previous gestational diabetes becomes pregnant again then the next pregnancy should always be considered high risk for subsequent diabetes and be tested for early in pregnancy.
Can gestational diabetes be prevented?
Gestational diabetes is more likely to occur if a person has certain risk factors but it can also occur without any identifiable risk. Risk factors are either fixed and are unable to be changed, called non-modifiable risk factors, such as your ethnicity, age or family history.
There are some risk factors, modifiable risk factors, can be changed. These include your weight, diet, and the amount you exercise. When planning for pregnancy, adjusting these modifiable risk factors are a great place to start to help reduce your risk of developing gestational diabetes. Some changes are around diet and weight management and is part of preparing for pregnancy.
If you have previously had gestational diabetes, there are key steps you can take to reduce your risk of gestational diabetes again.
What should I do next?
If you experience any symptoms of gestational diabetes or you have risk factors for developing gestational diabetes, it is important to be tested at 24-28 weeks gestation. Some people are at higher risk than others. If you are 25 years or older or have other risk factors for diabetes, you may require testing earlier in pregnancy. By diagnosing and treating gestational diabetes, it means you can decrease the risk of developing or delay any further health complications of gestational diabetes. These complications can affect both you and your child later in life, for example you are both at risk of developing type 2 diabetes. It is important to know that diagnosing diabetes should not rely solely on using a Hb A1c test.
Once you learn what your gestational diabetes status is, or if you already have gestational diabetes, the next most important step is to become educated. You can join the Gestational Diabetes Program to help you learn how to manage gestational diabetes and improve health outcomes for you and your child. The program is personalised and tailored, giving you more of the content that you want. The program also helps you to stay motivated and teaches you what changes you need to make.

