- Home
- Dr Sultan Linjawi
Type 1 Diabetes
Type 2 Diabetes
Prediabetes
Gestational Diabetes
- Diabetes Information
- Testimonials
How do you know if you have gestational diabetes and what are the symptoms

Treating gestational diabetes can greatly improve pregnancy outcome, for both mother and child. For many women, they’re able to achieve normal blood glucose levels through diet alone, however some women may require medications.
What is gestational diabetes?
Gestational diabetes explained simply
Elevated blood sugars often occur in pregnancy and are commonly caused by gestational diabetes (GDM). Mothers with Type 1 diabetes and Type 2 diabetes are also likely to have elevated sugars when pregnant. Around 1 in 5 pregnant women (20%) develop gestational diabetes.
Gestational diabetes explained in detail
In pregnancy there many hormonal changes that occur in the mother in order to facilitate the growth of a baby. Many of these changes are caused by hormones produced by the placenta. Some of these hormones cause the mother’s insulin receptors to become resistant to insulin. Insulin is a chemical that acts like a key, and when bound to the insulin receptor on a cell surface, opens a lock or channel so that glucose can move from the blood into the cells.
If a person is insulin resistant, then they require more insulin to open the lock and transport glucose out of the blood and into the cell. This is the same process that causes type 2 diabetes.
As the placenta grows during the pregnancy, more and more hormones are made and released to support the growth of the baby. This makes the mother more and more insulin resistant. At some point the mother may not be able to produce enough insulin to overcome the resistance, and if this occurs blood glucose levels rise.
Gestational Diabetes Content |
|---|
| Gestational Diabetes Program |
| Overview |
| Risk Factors |
| Symptoms |
| Diagnosis |
| Complications |
| Treatment |
| Diet |
| Monitoring |
| Tools |
| Mental Health |
| Prevention |
High glucose levels readily cross the placenta and expose the baby to sugars that are in the diabetes range, which can cause complications for the baby.
Can gestational diabetes happen to me?
All pregnant women may experience impaired glucose tolerance during pregnancy due to the hormones produced during pregnancy. Most pregnant women are able to make enough insulin to overcome the insulin resistance, but some cannot. For these women, gestational diabetes occurs when the pancreas can't increase the beta cell insulin production function sufficiently to overcome any insulin resistance associated with pregnancy.
Gestational diabetes often develops in pregnant women around the 24th to 28th week of pregnancy. This means that all pregnant woman should be tested for gestational diabetes at 24-28 weeks of pregnancy (except for those women who already have diabetes). Woman at high risk of developing gestational diabetes may have high sugars earlier in the pregnancy.
Typically, gestational diabetes goes away after the baby is born. However, women with gestational diabetes have a greater chance of developing type 2 diabetes later in life. 50% of women with gestational diabetes are likely to go on to develop type 2 diabetes in the future.
Children born to mothers with gestational diabetes, also have a higher chance of developing type 2 diabetes later in life. You can read more about genetics and type 2 diabetes for more information about how our genes can increase our risk of developing type 2 diabetes.
Gestational diabetes develops in pregnant women around the 24th to 28th week of pregnancy. This means that all pregnant woman should be tested for gestational diabetes at 24-28 weeks of pregnancy (except for those women who already have diabetes).
How common is gestational diabetes?
The number of women living with diabetes is increasing. The prevalence of gestational diabetes is related to the prevalence of type 2 diabetes (The Increasing Prevalence of Diabetes in Pregnancy). This means, that as the number of people with type 2 diabetes increases, so does the number of cases of gestational diabetes.
The International Diabetes Federation estimated that in 2017:
- 204 million women aged 20-79 years, have diabetes. This number is set to increase to 308 million by 2045
- 1 in 3 women of reproductive age lives with diabetes
- 21.3 million (16.2%) of live births had some form of hyperglycaemia in pregnancy. It was estimated that 85.1% were due to gestational diabetes
- 1 in 7 births were affected by gestational diabetes
- Hyperglycaemia in pregnancy is mostly prominent in low- and middle-income countries where maternal care is limited
What are the symptoms of gestational diabetes?
There are no obvious symptoms of gestational diabetes, as many of the changes that occur due to diabetes can be similar to the changes that occur due to pregnancy. However, it is important to understand and be able to recognise some of the symptoms of diabetes. If you are experiencing any new or unusual symptoms during your pregnancy, it’s important to visit your doctor.
Some of the general symptoms of diabetes in women include:
- Fatigue and irritability
- Excessive thirst, frequent urination, and dehydration
- Ongoing hunger
- Vaginal and oral yeast infections, and vaginal thrush
- Dry and itchy skin
- Cuts and wounds that don’t heal quickly
- Pain and numbness in your feet or legs
- Blurred vision
- Changes in weight
- Urinary tract infections
- Female sexual dysfunction
- Polycystic ovary syndrome
Why is screening for gestational diabetes important?
Identifying pregnant women with diabetes in pregnancy is important. Providing appropriate treatment to women with gestational diabetes can reduce the risk of complications to both the mother and the child.
Screening for gestational diabetes - how do doctors know when to test for gestational diabetes?
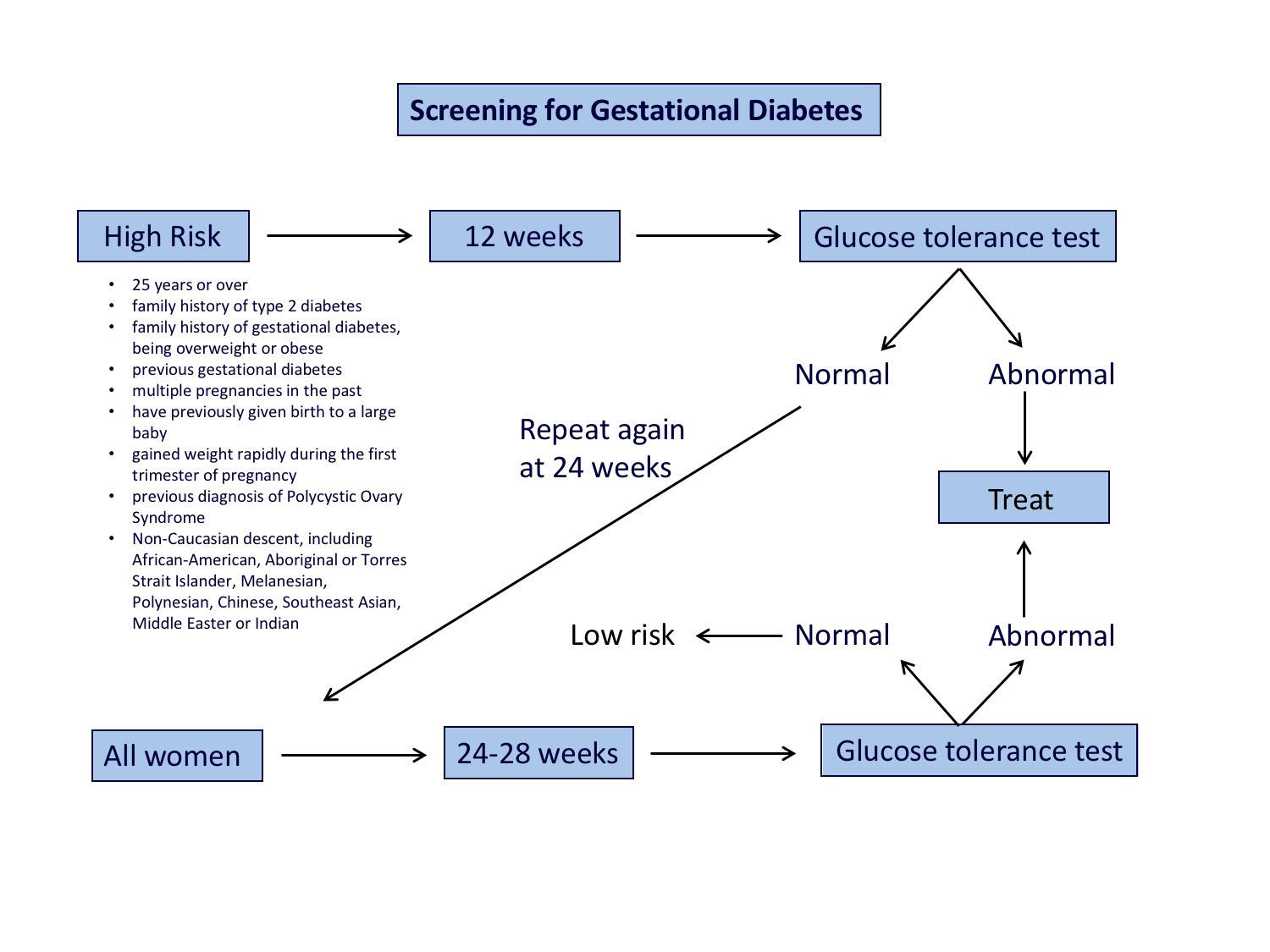
The image below provides an overview of screening for gestational diabetes.
How do you test for gestational diabetes?
All women should be tested for gestational diabetes at weeks 24-28 gestation, which is during the second trimester. If a woman is at a high risk of gestational diabetes such as being overweight at the beginning of your pregnancy; have previously had gestational diabetes; or a close family member (i.e. mother, father, or sibling) has diabetes, your doctor is likely to screen you earlier for gestational diabetes.
A pregnancy oral glucose tolerance test involves:
- fasting overnight (for at least 8 hours)
- initial blood test to test fasting glucose levels
- drinking a syrupy glucose solution containing 75 grams of glucose
- have a blood glucose test at 1 hour after drinking the glucose solution
- have a final blood glucose test 2 hours after drinking the glucose solution
The diagnosis of gestational diabetes is confirmed on high sugar readings at any of the following time points:
- fasting glucose value
- 1 hour glucose value
- 2 hour glucose value
What are the diagnostic criteria for gestational diabetes?
An elevation in blood glucose levels are diagnostic at either the fasting, 1 hour or 2-hour test. You only need one test to show abnormal blood glucose readings higher than normal values for each time point, to be diagnosed with gestational diabetes.
Diagnostic blood sugar levels for gestational diabetes
| Fasting glucose | 1 hour glucose | 2 hour glucose |
|---|---|---|
| 5.2 mmol/L or more | 10.0 mmol/L or more | 8.5 mmol/L or more |
| 92 mg/dL or more | 180 mg/dL or more | 153 mg/dL or more |
Read about how gestational diabetes is diagnosed for more information.
What should I do next?
If you experience any symptoms of gestational diabetes or you have risk factors for developing gestational diabetes, it is important to be tested at 24-28 weeks gestation. Some people are at higher risk than others. If you are 25 years or older or have other risk factors for diabetes, you may require testing earlier in pregnancy. By diagnosing and treating gestational diabetes, it means you can decrease the risk of developing or delay any further health complications of gestational diabetes. These complications can affect both you and your child later in life, for example you are both at risk of developing type 2 diabetes. It is important to know that diagnosing diabetes should not rely solely on using a Hb A1c test.
Once you learn what your gestational diabetes status is, or if you already have gestational diabetes, the next most important step is to become educated. You can join the Gestational Diabetes Program to help you learn how to manage gestational diabetes and improve health outcomes for you and your child. The program is personalised and tailored, giving you more of the content that you want. The program also helps you to stay motivated and teaches you what changes you need to make.
Interested in more information on gestational diabetes?
>Follow the links below to learn more about gestational diabetes.