- Home
- Dr Sultan Linjawi
Type 1 Diabetes
Type 2 Diabetes
Prediabetes
Gestational Diabetes
- Diabetes Information
- Testimonials
Ozempic (Semaglutide) is a new treatment for type 2 diabetes

What is Ozempic (Semaglutide)?
Ozempic is the brand name for a molecule used in the treatment of type 2 diabetes that is administered as a once weekly injection. The generic name is Semaglutide. It is not insulin. It comes in the form of 2 different disposable single use pens in either 0.25mg increments or 1mg increments depending on whether you are starting which, making it relatively safe and easy to administer.
Apart from lowering blood sugar levels, Ozempic can also aid with weight loss, appetite suppression and lower blood pressure levels. For more detailed information read the article below.
How does Ozempic work?
As Ozempic is 95% the same as human GLP-1 it works in a similar way to naturally occurring GLP-1 in the body and therefore has very similar effects including:
- increase release of insulin when blood sugar is elevated.
- Less glucose released from liver stores into the circulation.
- Decreased appetite.
Does Ozempic (Semaglutide) cause Weight Loss?
Yes. A side effect of Ozempic (Semaglutide) is weight loss, and increasinfly people are using Ozempic for weight loss if they have have type 2 diabetes. Doctors are also prescribing it off label for weight loss in those without diabetes.
There have been a number of studies examining the effectiveness of Ozempic (Semaglutide) in managing type 2 diabetes. These studies, the Sustain studies, also looked at the associated weight loss in patients using Ozempic. Across most of the studies the average weight loss was about 5kg.
Can Ozempic (Semaglutide) be used as a Weight Loss drug in people without diabetes?
Currently trials are under way looking at using higher doses of weekly Semaglutide as a weight loss drug in those with and without type 2 diabetes and the first of these was recently reported The Step 1 study. Based on these studies the US FDA has recently approved high dose Semaglutide 2.4mg weekly as a weight loss drug. It will be marketed a different product called Wegovy. Expect to see this available in the later part of 2021.
In this double-blind trial of 1,961 adults with a body mass index (BMI) of 30 or higher, adults on high dose 2.4 mg of weekly semaglutide (compared with the usual type 2 diabetes dose of 0.5mg or 1mg) lost an average 14.9% of baseline body weight after 68 weeks of treatment versus only 2.4% for a group on placebo and lifestyle intervention alone.
86% of people on semaglutide lost at least 5% of their body weight and almost 70% achieved a 10% or more weight loss, and more than half were able to lose 15% of their baseline body weight.
In total, adults on semaglutide treatment lost an average 15.3kg (33.7 lbs) after a year, while those in the placebo/lifestyle intervention group saw only a modest 2.6 kg (5.7 lbs) weight loss.
In addition to weight loss, semaglutide also caused greater reductions in waist circumference, systolic and diastolic blood pressures, HbA1c, fasting plasma glucose and fasting cholesterol levels.
Semaglutide (Ozempic) is the synthetic version of a naturally occurring human hormone, called Glucagon-like peptide 1 or GLP-1 that has been modified so that it is less likely to be broken down and therefore has a longer duration of action. It is administered once weekly.
Whether you have diabetes, or you don’t have diabetes, we all make GLP-1. It has become clear that GLP-1 is a really important hormone to help us regulate our blood sugar levels and probably our appetite and weight.

How does GLP-1 work and what is the mechanism of action?
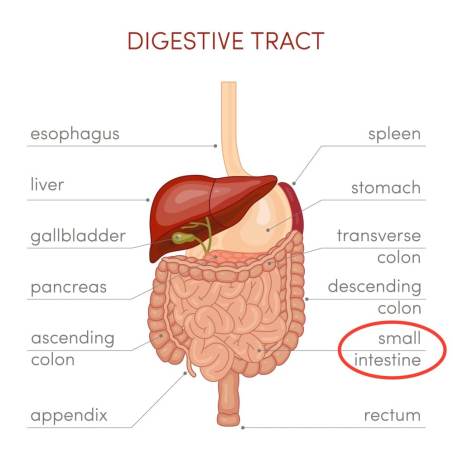
After we eat, GLP-1 is released from the small intestine.
GLP-1 has a number of actions in the body that improve blood sugar levels that include the following:
- Lowers blood glucose levels by stimulating the release of insulin from the pancreas. This process magnifies the release of insulin and is dependent on the blood sugar level. It is does occur if the blood glucose level is low and so GLP-1 medications do not tend to cause hypoglycaemia or low blood sugar levels.
- Reduces the amount of glucose that your liver is producing. Typically, the liver produces glucose, and it does this when you are in periods of starvation. So, the liver is a storage mechanism that can release sugar when your blood glucose levels are low and then store it when your blood glucose levels are high. In people with Type 2 diabetes, this process is completely impaired and the liver produces too much glucose.
- GLP-1 can cause you to feel full, so it increases early satiety. It does this by slowing gastric emptying, slowing the rate of food moving from your stomach into your small intestines. By doing this, the rate of absorption of nutrients into the blood stream is slowed, including glucose, which may reduce your food intake.
How is Ozempic (Semaglutide) different from GLP-1?
GLP-1 is a naturally occurring hormone found in all people. Ozempic (Semaglutide) shares 95% of the same structure as human GLP-1 but is synthetically manufactured. Semaglutide has been modified structurally to prevent it from being broken down by an enzyme in the blood called dipeptidyl peptidase-4 or DPP-4.
The formulation causes Ozempic to have a long duration of action and it is an example of a once weekly GLP-1. Another example of long acting GLP-1 is Trulicity (generic name Dulaglutide).
Drugs that block the action of DPP-4 are called DPP-4 inhibitors and these have been used in the treatment of type 2 diabetes for many years. By blocking the enzyme that breaks down naturally occurring GLP-1 they increase amount of GLP-1 in the body. (Dipeptidyl peptidase-4 (DPP-4) inhibitors for the treatment of type 2 diabetes mellitus). Examples of DPP-4 inhibitors include:
- sitagliptin (Januvia)
- valdagliptin (Galvus)
- saxagliptin (Onglyza)
- linagliptin (Tradjenta)
- alogliptin (Nesina)
If a person is taking a GLP-1 therapy they should NOT also be taking a DDP4 inhibitor.
What is the dose of Ozempic (Semaglutide)?
Ozempic starting dose
The starting dose of Ozempic is 0.25mg given a subcutaneous injection once per week for 4 weeks.
After this time, and if the person is able to tolerate the medication, the dose should be increased to 0.5mg weekly for at least 3 months when the effect should be assessed.
Ozempic maintenance dose
This is either 0.5mg or 1mg depending on the response to treatment.
The long term maintenance dose depends on whether the blood glucose levels are acceptable. Some people will be able to continue on 0.5mg weekly injections. For people who do not respond enough a further dose increase to 1mg is suggested. NovoNordisk the company that make ozempic are currently trying to have a 2mg dose approved for people with type 2 diabetes and this is currently under consideration by the FDA.
How many doses are there in an Ozempic (Semaglutide) pen?
The Ozempic (Semaglutide) injection pen comes in a 0.5mg or 1mg dose.
One 0.5mg Ozempic injectable pen would last 4 weeks.
Two 1mg Ozempic injectable pens would last 4 weeks.
Is Ozempic (Semaglutide) an Insulin?
Ozempic is not insulin but is a different type of diabetes medicine called GLP-1. It is a small protein like insulin (called a peptide) and because proteins are easily broken down by stomach acids, which would make the protein inactive, both insulin and Ozempic (Semaglutide) need to be injected under the skin. this allow the molecule to get into the body but bypasses the gut.
Is Ozempic available as a Pill?
Yes and no. Ozempic is the brand name for semaglutide once weekly injections. Semaglutide is available as an oral medication. It is exactly the same drug but as it is broken down by digestion a much larger dose needs to be administered. It is also less consistently absorbed and based on the data available it is probably not as effective in terms of sugar lowering or weight loss. For more information about read the following article Rybelsus (oral Semaglutide) Rybelsus (Semaglutide) - A new oral medication to treat Type 2 Diabetes.
How do you administer Ozempic (Semaglutide)?
Ozempic is contained in a disposable plastic pen which is based on the Novonordisk flexTouch pen. The process is exactly the same as administering insulin using the flexTouch pen.
For information about the flexTouch pen visit how to use ozempic pen.
Ozempic (Semaglutide) is administered once a week as an injection under the skin.
To help remember what day to take your Ozempic (Semaglutide), it is useful to have a reminder in your phone each week. It does not matter what day of the week to administer Ozempic (Semaglutide) so it is best to choose a day that best fits a person's lifestyle. For example, you might choose Sunday as your day to administer Trulicity. You can place a recurring alarm in your phone, so you don't forget. You administer it once every Sunday and that's done. Pretty simple!

What is the best area of the body to administer Ozempic (Semaglutide)?
The preferred site to administer the drug is the abdomen. Ozempic is only to be administered subcutaneously into the upper arm, thigh, or your abdomen. When administering into the same body region, e.g. your abdomen, choose a different injection site each week.
It’s important to change (rotate) your injection site within the area you choose to inject, for example your thigh. It is important to change the site with each injection to reduce your risk of getting pits in your skin or thickened skin and skin with lumps.
Here are some key points to remember when administering Ozempic:
- Do not use the exact same spot for each Ozempic injection
- Do not inject Ozempic where the skin has pits, is thickened, or has lumps – this can cause the Ozempic injection to not be effective
- Do not inject where the skin is tender, bruised, scaly or hard, or into scars or damaged skin
How often is Ozempic (Semaglutide) administered?
Ozempic is administered once per week and ideally that is on the same day each week.
What do I do if I miss a dose of Ozempic (Semaglutide)?
If you miss your dose of Ozempic (Semaglutide), you can administer it as soon as possible within 3 days after the missed dose. After this, you can go back to your regular dosing schedule of once per week.
If there are less than 3 days until your next scheduled dose, don’t take your missed dose. Take your next scheduled weekly dose and return back to your regularly scheduled weekly dose!
What are the side effects of taking Ozempic (Semaglutide)?
Although Ozempic (Semaglutide) is an effective medication for the treatment of type 2 diabetes, there are a number of Ozempic (Semaglutide) side effects (Trulicity (Dulaglutide): A New GLP-1 Receptor Agonist Once-Weekly Subcutaneous Injection Approved for the Treatment of Patients with Type 2 Diabetes). Below is a list of the Ozempic (Semaglutide) side effects, and includes common side effects and serious side effects.
Common side effects of Ozempic (Semaglutide)
The most common side effects of Ozempic (Semaglutide) injection are:
- nausea
- diarrhoea
- vomiting
- abdominal pain
- decreased appetite
These gastrointestinal side effects may be experienced by over 10% of people using the Ozempic injection pen. The feeling is similar to the sensations felt if a person really over eats.
These gastrointestinal side effects will subside in most people within 8-12 weeks and semaglutide is well tolerated in the long term.
Serious side effects of Ozempic (Semaglutide)
Ozempic (Semaglutide) may also cause more serious side effects including:
- inflammation of the pancreas
- hypoglycaemia
- allergic reactions
Subscribe to Receive One of Our Helpful Free Guides
Click the guide that would be the most useful
Does Ozempic (Semaglutide) cause thyroid cancer?
The simple answer is no, GLP-1s do not cause thyroid cancer in humans.
Early studies demonstrated that when rats were treated with a different GLP-1 therapy in high dose many developed a very rare and lethal thyroid cancer called medullary thyroid carcinoma. Rats have very high levels of GLP-1 receptors in their thyroids. These are not present in human thyroid cell.
The early concern that GLP-1 causes thyroid cancer has lead to extensive investigations and studies looking at this issues and to date there has been nothing to suggest a concern despite millions of people being treated with GLP-1 therapies around the world. It is not recommended to use GLP-1 therapies like Trulicity and Victoza (liraglutide) if there is a family history of medullary cell carcinoma of the thyroid or Multiple Endocrine Neoplasia Type 2 (MEN 2).
Who can use Ozempic (Semaglutide)?
Ozempic (Semaglutide) is designed to be used by people with type 2 diabetes. In combination with diet and exercise, Ozempic can help to improve glycaemic control. It is not approved for use in people with type 1 diabetes.
Is Ozempic (Semaglutide) ok to use during pregnancy?
Currently, Ozempic (Semaglutide) is not recommended for pregnant women. Other types of medications are used to treat diabetes in pregnant women.
If you have type 2 diabetes and are looking to start a family or add a new member, it is recommended that prior to conception and throughout pregnancy, your blood glucose levels and HbA1c levels are kept as close as possible to the target goals. These goals may be set by your doctor.
Please see the following articles for more information and diabetes and pregnancy:
- Pregnancy diet and diabetes: Preparing for pregnancy
- Diabetes and diet in pregnancy
- Medications in pregnancy: Safe or unsafe?
- Key steps to reduce having gestational diabetes again
Do I have to Ozempic (Semaglutide) with food?
You can administer Ozempic (Semaglutide) with or without food (Trulicity (Dulaglutide): A New GLP-1 Receptor Agonist Once-Weekly Subcutaneous Injection Approved for the Treatment of Patients with Type 2 Diabetes).
Can I drink alcohol with Ozempic (Semaglutide)?
You can drink alcohol with Ozempic (Semaglutide) although there are some people who find they enjoy drinking less when taking it. This is particularly with large volume gassy drinks like beer.
Do I have to change my diet if I use Ozempic (Semaglutide)?
If you have type 2 diabetes, making lifestyle changes, for example exercising and eating a healthier diet, is very important.
For ideas on how to reduce the carb content of some of your favourite foods, the article How to reduce carbs in your diet has many great ideas that won’t leave you missing out on flavour.
DO YOU WANT TO GET YOUR DIABETES UNDER THE BEST CONTROL?
Click the program that best describes your situation.
Does Ozempic (Semaglutide) need to be refrigerated?
Yes. If you have excess Ozempic (Semaglutide) injectable pens at home, they need to be stored in the fridge.
The best place to store your Ozempic (Semaglutide) pens in the fridge, is on the top shelf of the fridge door. The butter compartment is usually the safest place. You shouldn’t store your ozempic pens in the coldest part of your fridge. If the ozempic injectable pen becomes too cold, then the semaglutide will degrade, making it less effective, leading to higher blood glucose levels.
Long term storage should be in a fridge between 2-8℃ or 36-47℉. Once the pen is used it can be safely used for 56 days if maintained at a comfortable room temperature of 15-30℃ or 59-86℉.
How long does it take for Ozempic (Semaglutide) to start working?
It may take Ozempic (Semaglutide) up to 5 weeks to start lowering your blood glucose levels but the maximum effect will not been seen for 3-6 months.
How long does Ozempic stay in your system
If a person takes Ozempic for a few months and then stops it then it will take about 5 weeks to completely clear the system.
As a general rule with medication if a drug is taken daily then it takes 5 days to get to a steady level and 5 days to clear the system. If a drug is taken weekly then it is 5 weeks to get in and 5 weeks to clear.
Ozempic vs Trulicity (Dulaglutide)
The Sustain 7 study compared the treatment outcomes of Ozempic with Trulicity. Both of these drugs are once weekly GLP-1 analogues used in the treatment of type 2 diabetes.
Ozempic compared to Trulicity led to:
- lower blood sugars based on HbA1c by about 0.3%(-1.4% vs -1.1%).
- Twice as much weight loss with Ozempic (4.6kg-6.5kg depending on dose).
- More people had HbA1c below the 7% to suggest safer sugar levels.
- People using Ozempic had more nausea compared to Trulicity.
Ozempic vs Bydureon (Exenatide ER)
The Sustain 3 study compared the treatment outcomes of Ozempic with Bydureon (Exenatide ER). Both of these drugs are once weekly GLP-1 analogues although Bydureon is based in the Exendin molecule rather than human GLP-1) used in the treatment of type 2 diabetes. Exendin is only 55% similar to human GLP-1.
Ozempic compared to Bydureon led to:
- lower blood sugars based on HbA1c compared to about 0.6% (-1.5%vs 0.9%).
- Weight loss with Ozempic was 5.6kg vs 1.9kg with Bydureon.
- More people had HbA1c below the 7% to suggest safer sugar levels.
Ozempic vs Victoza (Liraglutide)
Both Ozempic and Victoza are very similar drugs with both based on human GLP-1. There are some small differences that extends the action of Ozempic and makes it a once weekly treatment for type 2 diabetes as compared to Victoza which is given daily.
So far there have been no direct studies comparing Ozempic and Victoza and it is unlikely that there ever will be as both drugs are made by the same company, Novonordisk.
There are some indirect comparison used which suggests Ozempic may be more effective and this is based on Ozempic being more effective than Trulicity while Trulicity and Victoza were about the same in the AWARD-6 study.
Ozempic (Semaglutide) alternatives
The following drugs are all based on the GLP-1 or Exendin molecule:
Administered weekly
- Ozempic (Semaglutide)
- Trulicity (Dulaglutide)
- Bydureon (Exenatide ER)
Administered daily
- Victoza (Liraglutide)
- Byetta (Exenatide)
- Lyxumia (Lixisenatide)
- Rybelsus (oral Semaglutide)
What are the other effects of Ozempic (Semaglutide)?
Did you know that GLP-1 has many effects in the body?
As we’ve discussed above, GLP-1 is a hormone that is released from our small intestines in response to food. When GLP-1 is released, it binds to specific GLP-1 receptors. These receptors can be found in various areas of the body (GLP-1 Receptor Localization in Monkey and Human Tissue: Novel Distribution Revealed With Extensively Validated Monoclonal Antibody), including in the:
- pancreas
- stomach
- kidney
- lung
- heart
- skin
- immune cells
- hypothalamus
Looking for more diabetes videos?
Check out our latest diabetes videos for more great content.
Video Transcript for Ozempic video
Today, I would like to talk about Ozempic and explain how Ozempic or Semaglutide works, what the effect is and what you can likely expect, the side effects and essentially how to take it and get the best and the most out of it.
My name is Dr Sultan Linjawi. I'm a certified Diabetes Specialist and Endocrinologist and this is what I do for a living. I provide education around new diabetes treatments and old diabetes treatments, to people around the world.
So let's talk about Ozempic, or Semaglutide. So Semaglutide (Ozempic) is a once weekly injection for people with diabetes. It is something called a GLP1 analogue and I'll explain a little bit what a GLP-1 is.
But in essence it looks very similar to a naturally occurring chemical that we all produce that helps us regulate our appetite as well as our blood sugar levels and this treatment is for people with Type 2 diabetes where it has been tested and investigated fairly heavily. It is not approved for people with Type 1 diabetes and shouldn't be taken in women who are pregnant or breastfeeding and it is ill-advised at the moment to be using it in children.
So what is a GLP-1?
Well GLP-1 is an extremely powerful chemical that is produced in response to eating by our gut and it does a number of things, but there are four main actions.
So the first is that when the chemical is released it circulates into our system and it gets to our brain and there it leads to reduced appetite. It is the thing that people experience when they have eaten too much where suddenly they feel they are just overfull.
That sense of sickness, or fullness, that you might feel if you have gorged yourself is actually GLP-1 hitting the brain and saying that is enough. Now, some people seem to produce fantastic GLP1 responses that are really effective. Generally, people that are thinner, they stop eating a lot more quickly.
But we know that in people with Type 2 diabetes that sense is often impaired
and if you give someone GLP-1 you can switch off the appetite to some extent
and achieve some weight reduction.
Now how else does it work in the body?
Well, in the liver, it reduces the amount of glucose, or sugar, that is released by the liver. The normal situation for a person would be to release sugar into the circulation unless you don't need it. But in Type 2 diabetes, there is impaired release of glucose out of the liver. Continually the stores are being released into the circulation even though the blood sugar level is elevated.
So the third mechanism of action is around slowing stomach emptying and slowing what we call gastric emptying that process leaves food in the stomach for longer therefore there is less necessity to go looking for food and finally, the action is around the effect on the pancreas where GLP-1s both increase the amount of insulin that is produced as well as increase the amount that is released. And the interesting thing about it is that that is predominantly when the blood sugar is elevated.
In other words GLP-1s and there are a range of these treatments all have an effect which is predominantly around high sugars and if the sugar becomes low, the effect is switched off, and it is the reason we see very low rates of low blood sugars so called 'hypos', or hypoglycemic episodes that occur with GLP1 treatments.
So if you are on Ozempic or Semaglutide what dose should you use?
Essentially there are two doses that are prescribed and talked about.
One is 0.5mg and the other one is 1mg. And the way we take it, well this is how you start taking it. In the clinical trials, it was a weekly injection and they started at 0.25mg a week and that was for 4 weeks.
At the end of 4 weeks, predominantly that was around getting used to the drug, at the end of 4 weeks, the dose was increased to 0.5mg weekly. And for many people that is an extremely effective dose. In fact for some people, the lower dose is still going to be highly effective in terms of 0.25mg and there may not be a need to increase the dose even though the clinical trials suggested that was what needed to happen.We do not know what the actual effect of 0.25mg is.
Now if 0.5mg isn't enough and you have waited some time and the blood sugars are still not where they need to be, then we do have the option of increasing it to the 1mg dose.
So it is a step process, 0.25 initially for 4 weeks to get used to it, then 0.5mg, and if that is the dose for you, fantastic.
If you need escalating further, then up to 1mg. But I want to say this, because I think it is important. Ozempic (Semaglutide) will take 5 weeks to get going and get into your system. It won't reach, what we call steady state, until that time. Its main effect won't be felt for 12-24 weeks.
So if you think, I'm going to take this drug and in 2 or 3 days my sugars are going to be perfect that's not how it works. So you have to wait for its effect to have so you can make those judgments about when you need to increase the dose and if you stop it, it clears the system or the body, in about 4 or 5 weeks.
So how does Ozempic (Semaglutide) compare to other GLP1 therapies?
Well I think it is just worth mentioning there are a lot of GLP1 treatments available at the moment and some of them you will be familiar with, there are weekly versions and daily versions.
The weekly versions that we are looking at are things like Trulicity, which is called Dulaglutide, or Bydureon, which is known as Exenatide Extended Release and then we have daily versions and daily versions would be Liraglutide, or Byetta and maybe the only other agent that is used a bit is Lixisenatide. So we have quite a bit of options in terms of GLP1 treatments and most of those options are being tested and looked at.
So the first study I want to show you, is this one.
This was looking at whether or not Ozempic worked, and it was comparing Ozempic to a placebo, so a dummy injection and across the whole of this image, the light blue bars are the low 0.5mg dose of Semaglutide (Ozempic) and the dark blue bars are 1mg. And you can see that both of the Ozempic (Semaglutide) doses, lowered HbA1C by around 1.5-1.6% compared to placebo incredibly effective.
Compared to Bydureon or Exenatide Extended Release the 1mg dose lowered the HbA1C by about 1.5% compared to Exenatide at 0.9% so there was about a 0.6% reduction but Ozempic was superior.
They compared it to insulin. In this case insulin glargine or Lantus. You can see whilst Lantus was effective at lowering the blood sugar by about 0.8% of an HbA1C again there was superiority in the 0.5mg and 1mg dose of Semaglutide (Ozempic).
And the only drug that really got close, and it really did get very close, and is a reasonable comparison is Trulicity, or Dulaglutide. And there are two different doses of Trulicity as there are two different doses of Ozempic but to both ends it looks like Ozempic was superior by about 0.4mg. So that is impressive. Because Trulicity is a very, very effective drug for many, many people.
What about weight loss?
We talked about the fact that these drugs are exceptionally impressive at weight reduction and in fact out of all the drugs that we have to date in the GLP1 category Ozempic (Semaglutide) seems to be the most effective around weight reduction. And if you just look at this graph, anything above the line, is a weight increase.
So you can see that in the middle there with the little green mark there around insulin glargine (Lantus) which put on a bit of weight. But across all the other drugs, and the other trials, there was weight reduction and consistently it looks like there was a weight loss of between 3.5kg - 6.5kg favouring Ozempic with the bigger weight loss seen in the higher dose.
So what are the side effects of Ozempic(Semaglutide)?
Well, the common side effects are nausea, diarrhoea, vomiting, abdominal pain, and decreased appetite. And that is what was reported, but in fact if you talk to people who are using it, it is that sense of fullness, that queasy feeling that you have if you have eaten too much. Imagine going to a wedding and just stuffing your face and then someone saying "would you like another dessert?" and just thinking no I can't eat anymore.
That is the sensation that you get with GLP1 therapies and it is experienced by about 10-20% of people but the vast majority of these symptoms settle after around about 8-12 weeks in most people and if somebody were in a situation where they felt nauseated there is no reason that they need to escalate from 0.25mg up to 0.5mg until that nausea has settled.
Because it is a very powerful drug and it would be a shame if we gave up on it because the side effects were bad in the first week or two and we didn't find a way to persist.
Now there are a few serious side effects that are noted.
So there was a concern with a GLP-1s around inflammation of the pancreas that is extremely rare, low blood sugars are unlikely, but possible, and of course, there are allergic reactions.
So there is Ozempic (Semaglutide).
A new treatment that is being launched all over the world that is for people with Type 2 diabetes, that seems to not only lower blood sugars but also in lowering blood sugars leads to some weight loss.
There is some good evidence also that in people who have cardiovascular risk factors, in other words, people who are either susceptible? to heart attacks and strokes or people who have had one in the past, this reduces the likelihood of having a further event by around 25-26%.
That is in common with a number of other GLP-1 drugs.
So these are really powerful agents that are really helping us, as healthcare professionals, provide great care and outcomes for people with diabetes and certainly a great tool if you have diabetes to help you moving forward because with the benefits of weight loss and the reduction in blood sugars being so powerful and the potential benefit of reducing heart attacks and strokes this is part of the future of diabetes that is here right now.
More Articles on Diabetes Treatments
For more information about different Diabetes Treatments, please follow the links below.
Oral Medications for Diabetes
- Starting on Metformin. What you need to know.
- Benefits of Metformin… A Wonder Drug?
- Metformin in Pregnancy. Is it safe?
- Metformin and diarrhoea.
- Vitamin B12 deficiency and diabetes.
- What is an SGLT2 inhibitor? It's a novel way to lower blood sugars, lose weight and maybe live longer.
- Rybelsus (Semaglutide) - A new oral medication to treat Type 2 Diabetes.
---
Insulin for Diabetes
- What is Ryzodeg insulin and how do I use it?
- Fiasp insulin. Fast acting insulin aspart.
- Managing Diabetes with Insulin: Is it necessary?
- Lantas. Solostar insulin glargine.
---
Injections for Diabetes
- What is Trulicity (Dulaglutide) and how does it work?
- Ozempic (Semaglutide) is a new treatment for type 2 diabetes.
- Xultophy 100/3.6 - Type 2 diabetes medication - Benefits, Side Effects and How to Use It.
- What is glucagon and how can a glucagon kit help someone with diabetes?
---














